Almost a year after the Coalition Government made drastic changes to how disabled people and their families could use Individualised Funding we finally have a public consultation. The Consultation began a couple of days ago, and will continue until 24 March with a series of in-person and online workshops , with additional opportunities for individuals to make submissions based on a series of questions via the disability support services website. The consultation and workshops were announced about a month ago, and on the whole have come with access provision and options for how to participate.
The Consultation is asking the disability community to feed back on Two Topics related to Individualised (flexible) Funding:
Topic 1 – Improving the way the needs of disabled people are assessed, and how support is allocated (this means how much money is going to be allocated to who, and how it is going to be calculated)
Topic 2 – Accessing flexible funding, and how it can be used (how the disabled person and/or the family carer or agent can use the budgeted money)
You can read more about the consultation here: https://www.disabilitysupport.govt.nz/consultation
While it is with relief that the disability community are finally being consulted, there is much skepticism from the disability community about how the information we provide will be used, if at all. There is a vibe that the consultation is a formality with a pre-determined agenda. With the questions targeted to drive our answers towards outcomes that are what the government has already decided on. We have been here before. The saying ‘this is not our first rodeo’ comes to mind. Many disabled people, their families, providers and organisations have provided advice, options and suggestions for solutions to the ever changing Disability Ministers and public service administrators who hold the key to distributing funding from a budget that doesn’t match the needs of the people. For this ‘consultation’ I hope our community can stand up and give frank, honest and aspirational ideas to drive the conversation in a direction that will meet their needs and wants.
This past year we have heard loud and clear that the budget provided to support the disabled will not be increased to match the needs of the disability community. It’s true that there was an increase in the budget last year, but like the previous governments, the increase has not met the need in growth of those with disability. There has been a constant increase in numbers needing DSS’s over the past decade, and this is a continuing upward trend. For many years it has been like to trying to feed a family of four, when you only have a budget to feed two – it doesn’t matter how many different ways you try to stretch it, someone is going to walk away with an empty stomach or a nutritional deficiency.
If we use a food budget as an example – when there is not enough money we are forced to make choices:
- Do we go without red meat or reduce the amount or type of meat we eat? For Disability funding, do we restrict the hours of personal care and support workers?
- Do we eliminate the snacks between meals? ie. Do we stop respite breaks for family carers? I mean are snacks essential? Do they make a difference?
- Do we stop eating a wide range of foods and replace it with cheaper and less healthy options? While you might want to buy some Freshly squeezed juice, the Coca-cola is much cheaper. i.e. instead of freedom to choose items that improve wellbeing and sustainability, we give a list of what is on the menu today – too bad if you don’t like it or if it is not good for your long term health.
- We can only have the cheapest fruit and veges e.g. bananas, apples, potatoes and cabbage – everything else is off the list, ie. you can have a sensory item as long as it is small, but not something that you actually want eg. a trampoline. Don’t expect grapes or avocado!




- When the food budget has run dry, we choose who will get fed first? Will it be Mum, Dad, the spouse, the children, the extended family i.e. those with the highest needs might get some funding, but if you have Autism you miss out. How do we pick who is most valued and needy?
- You definitely can’t go out to eat or buy a takeaway, ie. you can’t spend money on travel to get there or expect to have a break from cooking, ie. you should stay home as travel should only be within your region.
- You would like to buy soy milk or gluten free products because you know that it will improve your wellbeing, but it’s not available ie. you need speech therapy, physio, OT support but that is supplied by a different government department and so you can’t use the money you have to buy it from another department. You can see it but it is out of reach.
The list could go on – there were so many ways the 18 March 2024 affected people differently. It wasn’t just the items on the table for Individualised Funding that went, it was also the restrictions around residential care and equipment and modifications that were implemented. The Disability Community has been hurting for almost a year from these changes and waiting to have their say. Now, we are being asked to have our say on these two topics but once again we are being coralled into options to choose from that the Taskforce has designed based on themes and feedback from organisations, providers and earlier feedback and complaints following the changes.
In the food scenario, every person and family with a limited food budget will make choices about how they stretch their money to meet their families needs. Some will happily go without meat, some don’t like vegetables, so they won’t mind missing them, some will make a vege garden or have families who give them food, some will choose to eat less or miss meals so that they give more to their children. Just like people making choices about their food and how to feed their family there will be a variety of answers to the questions posed. The disability community will not all want the same things – the needs of the disabled person with a physical disability versus a sensory impairment vs learning disability versus complex disability versus the family carers needs will all need to be taken into account. Disabled people and their families are unique. We are not a ONE SIZE FITS ALL community. We are not even a ONE SIZE FITS MOST. What I believe we need most is to have CHOICES to meet our needs. For one person, this is being able to pay a support worker, another it is buying an item, another it is to take a rest, another it is to use a provider’s service etc.
Organisations I am involved with have been using as many avenues as possible to influence change and to have at the minimum the previous flexibilities reinstated. The Complex Care Group, made a proactive submission at the end of last year regarding specific needs for assessment of those in the complex care group, based on what our members have told us over time. At Disability Connect where I work part time, we met last with the Minister of Disability, Louise Upston and the head of the Taskforce, Chris Bunny to discuss the needs of our communities (it was not a consultation) – I did not come away with warm fuzzies. Disability Connect will also be making a written submission, to incorporate feedback we have received over the year and from our survey. Via the Whaikaha Strategic Advisory group where I represent the Family Whanau Network we have been urging reinstatement of flexibility, accessible consultation and many of the other things our communities are asking for any way we can. Many, many organisations and individuals have been advocating for their communities tirelessly via protests, media and submissions to both Whaikaha and DSS. Yet we don’t seem to be effecting any change.
Like others affected personally by the changes I will make a personal submission and also attend a workshop. I have been to a couple of protests this past year, written to both Hon Penny Simmonds and Hon Louise Upston, written, ranted and raved about the issues. But we still need to do more – and the more means participating in this consultation. I have learnt over the years that we need to keep repeating our thoughts, ideas and solutions to the government and government departments because there is always turnover of staff and Ministers who are reading what we submit. It often feels like each time we have a change all of the feedback previously given is just shelved somewhere collecting dust. It feels like no-one is reading it, or taking action from it. Or we are being consulted BUT they are never going to make changes because the budget is not going to be increased. But, we need to continuously present our ideas if we want to improve our situations and regain hope. While it feels like banging our head against a brick wall – we must remember how far we have come from 30 years ago. We must keep advocating for our disabled people, ourselves (as family carers) and for the next generations.
For me, one positive of this process (yes there might be one) is that the Independent Review showed the under-investment in Disability over the years. It illustrated that there is a greater need than the budget allocated. It highlighted that the Ministry of Health is not providing enough therapeutic supports and we are having to spend our IF on items that should be provided by other departments. It highlighted that Education is also not providing what it should for our disabled people. It highlighted that many of the issues have been created by inefficient systems and contracts, as in the case of residential care. Even if you don’t like or agree with this Government’s statements around disability and how they have mishandled the ‘pause’ on funding – they have at least shone a light what we all suspected and given us some data to use. Successive governments, across many years, have not allocated enough funding to meet the needs of the growing disability community. Not only have they not allocated enough funding, the systems and processes meant to be supporting the disability community are stuffed. (I was trying to find a better word to use there, but really stuffed is appropriate).
In the 21 years I have been a mother and carer to my son, I have wept many tears and this past year has been seriously challenging because not only did we have the reductions and pause, but a transition out of school and into the adult system. It felt like we were being attacked from both sides. The thing is, that our joureny is not just this past year but it began with a little over 2 years living in Starship hospital before we could have our son living in the community. We left Starship with Carer Support and overnight caregivers for our son who had complex disability and high health needs, including using a tracheostomy and BiPap. We were critically under resourced, but we were desperate to go home. Since then, I have advocated passionately to receive as much as possible for our son in order to hold our family together. Over the years we have been resourced using different funding streams and eventually we received combined disability and health funding which is now distributed via Individualised Funding.
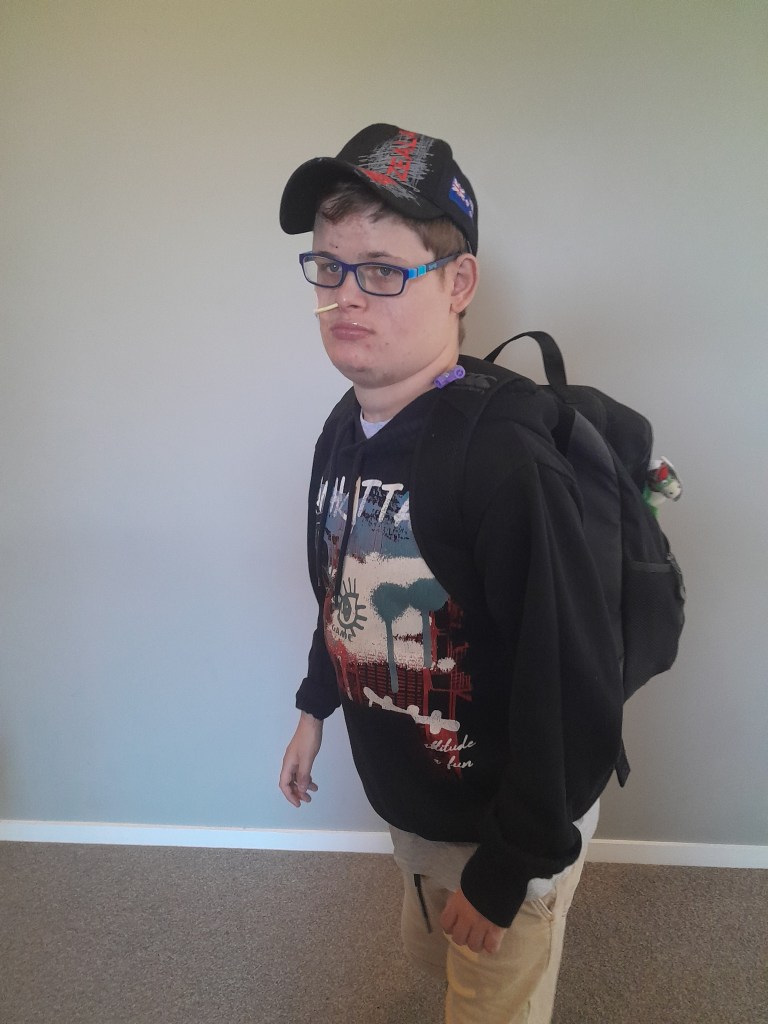

Photos: Mitchell ready for his last day of school and Mitchell and I at a recent family wedding.
I have shouted at numerous people on the end of a phone (something I am not always proud of). I have written many letters to MP’s, our NASC, anyone who might listen or be influenced. We have always, always challenged the options we have been given. Every needs assessment I have agonised over whether we will receive enough support to sustain our family. We have compromised our own financial situation/our work choices/our lives in order to meet the needs of our son. There have been many awful needs assessments, but this past year, was one of the worst as far as uncertainty and advocacy went.
In June, the DHB cut our funding substantially (this is for the overnight cares) without any justification. It has taken almost 6 months to get a revision, and it still does not match the previous year’s allocation, even though the needs increased – not decreased. Our DSS funding was rolled over, but as our son left school in December, this no longer meets either his or our needs. We had advocated for an increase in funding to meet the extra 25 daytime hours where he needs supervision and would not be at school. Although he receives Very High Needs (VHN) ORS funding and this can be transferred to MSD, it does not provide one on one support. We receive a very large funding package to enable our son to live at home and not in state care or a hospital – but that funding package comes with a huge amount of administration, recruiting support workers, training support workers, doing a payroll for 5 or 6 employees, managing a team of people in our home – this is recognised by our government with a $300 honorarium to a parent. For the work, I do for this alone (without caregiving) I must be earning around 0.5 c per hour. This is not ‘parent’ work, and I don’t want an agency doing it (that is not my solution), we have used providers and agencies who sent us incompetent, untrained, inconsistent support who upset my son by not being able to understand him. I am adamant that what works for one family or one disabled person does not mean it works for another. It comes down to flexibility.
We have been declined from two providers of VHN day programmes as he is considered too complex and challenging, and they do not have the staff to support him. We are waiting now trying to find a suitable placement for at least 2 days of 9 to 3 pm per week to give him some routine, as he gets up each day and signs that he wants to go to school. We started the ‘out of school transition process’ over a year ago. We followed the process, researched options, did all the right things, only to find that we don’t fit the box. It’s not even as though day programmes are terribly attractive, but how do you help someone fill their hours when their life is full of challenges and they are not going to work? I would love to hear solutions from the community or from the Minister who seems to think only those who are productive are valuable members of society.
Mitchell is no longer eligible for facility based respite care at Wilson Home as he has ‘aged out’ and now our only option is within aged residential care, should we need respite for him out of our home. While we have come up with arranging a once a month break at a caregivers home, we can only do this by paying for this out of our personal finances – which means we need to work more, and this is almost impossible when you are constantly trying to balance the support hours with paid work outside the home.
Our case, is just one of many. The funding isn’t enough, the services don’t match the needs of our son, and we are left as a family to carry the load. It is what we do. We get on with it. We make do. We cancel any plans we had – and just do our best. Earlier this week when a support worker canceled for a bereavement we shared staying up overnight to supervise. Phil and I taking a couple of hours of sleep each in turn. The night is never smooth – after not having a bowel motion for 3 days, suddenly we are delivered with 4 big BM’s which involve multiple changes, clean ups and attention. It’s not just the BM’s it is the constant request of who is coming next? Or listening to Pete the Cat or the Wiggles on repeat ALL night. Eventually it wears you out. It makes your mind explode. You envy other people who don’t deal with this. Finally, your son sleeps at 6.30 am. But that doesn’t mean you can sleep. Phil goes to work after a total of 3.5 hours sleep, 2 hours from 10 to midnight, and 1.5 hours from 6 am to 7.30 am. I have had 6 hours sleep, from 12 to 6 am, but even that was broken, as one part of the night it required two of us to settle Mitch from a meltdown and a BM.
I can’t explain to someone in a Ministry just how difficult and tiring it is to be hypervigilant all day – everyday. I can’t get through to those who make policy decisions that an adult with the mind and behaviours of a child because of intellectual disability is not going to go out and find a job. I can’t get through to policy makers who think natural support means being oncall 24/7, changing your adult child’s nappy, making and administering medications, putting down an NG tube daily. There is nothing natural about that. Many of the families with complex children and adults do cares like a nurse performs with no holidays, no downtime, no lunchbreak, no-one to cover when they are sick. It truly feels like those making policy and decisions just don’t get it. Even when we have support workers, we are on call 24/7 as back up, as a 2 on 1 when needed.
I am afraid that the feedback from the consultation will go nowhere BUT I also know that unless we keep standing up and sharing our realities nothing will even have a chance to happen. I urge everyone who is disabled or caring for a disabled family member to stand up for our rights. A right to flexible and adequate funding. Flexibility is important and flexibility isn’t just 2 choices given to us in the consultation. It’s CHOICE AND CONTROL. As a community lets get some fire back in our bellies (remember how we felt on March 18), rally and tell the Taskforce what we want. Not just what we need – but what we want too.
Being flexible means – “able to be easily modified to respond to altered circumstances”. We don’t want prescriptive funding that has to match an outcome plan that is out of date 3 months after it is written. We don’t want to have to use providers – but if you want to that is also okay. We want to be able to use the funding allocated by a needs assessment (because it is needed), however we choose – this is what flexible means. We really need to return to aiming high with the Enabling Good Lives approach. The Government, while not giving any funding to EGL have stated that it’s still an approach we can use – and use it we must.
Other than that, if the upcoming budget for 2025/6 is not increased there is simply no way everyone is going to be fed. That’s my rant for the day. I’m off to start working on my submission.
Take care and be safe.
Cherie